Gonarthrosis (knee arthrosis)
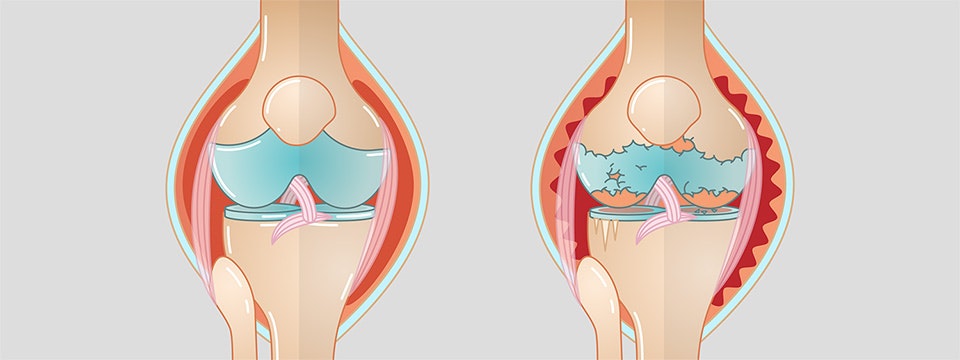
Gonarthrosis, also called knee arthrosis, is progressive wear of the cartilage in the knee joint. Arthrosis-related breakdown of the cartilage material reduces the stability of the knee, and may cause severe pain and restricted movement.
Learn more about gonarthrosis in this article. What exactly is gonarthrosis and what are its symptoms? What causes gonarthrosis? What are the possible treatments and therapies? And much more …
What is gonarthrosis?
The term gonarthrosis (ICD code M17) consists of two words. Gony, the Greek word for knee, and arthrosis, a disease in which cartilage material in the joints deteriorates due to wear. Accordingly, gonarthrosis (knee athrosis) is a disease of the knee joint, caused by the wear of the cartilage between the thigh and the lower leg. The cartilage stabilises the knee, and protects it against damage due to friction against the bone. The decrease in cartilage may cause restricted movement and severe pain.
Gonarthrosis is one of the ten most common diseases in the world (Kiselev 2008). According to recent studies, 15-16% of 50 to 54-year-olds show signs of gonarthrosis. For the 70 to 74-year-olds, this proportion increases to 36-40% (Stöve 2018).
In general, a distinction is made between two types of arthrosis. Primary arthrosis is caused by genetic predispositions. However, not everyone who has this genetic predisposition will develop the disease. Secondary arthrosis is caused by external impact, such as injuries due to accidents, misaligned legs (knock knees/bow legs), or constant stress at work.
Arthrosis is often confused with arthritis in everyday language. Arthritis is a generic term for inflammation-related joint diseases. These include, for example, infection-related arthritis and rheumatoid
arthritis. Gonarthrosis may sometimes cause inflammation also. In this case, it would also be called arthritis.
Causes of gonarthrosis
In most cases, gonarthrosis is age-related wear of the cartilage in the knee joint. The main reason for this wear is that the body's ability to repair minor damages decreases over time.
Arthrosis may also occur at a younger age due to genetic predispositions or knee overloading. Stress-related causes of gonarthrosis include:
- obesity
- misaligned legs (e.g. knock knees, bow legs)
- knee injuries (e.g. a meniscus rupture)
- permanent stress in one’s daily routine (e.g. craftsmen)
- high-impact sports (e.g. football)
People with a genetic predisposition for gonarthrosis may not necessarily suffer from any complaints. The predisposition may exist for a lifetime without causing symptoms. The causes of gonarthrosis are extremely diverse. Sometimes, there is no specific reason. In this case, the disease is called idiopathic gonarthrosis.
Symptoms of gonarthrosis
Gonarthrosis usually manifests itself as pain and restricted movement of the knee joint, but symptoms do not necessarily have to be noticeable. In the early stages of the disease, those affected usually only feel a slight pain when moving the knee. The pain often disappears after a few steps.
If the gonarthrosis persists, all of the cartilage material will have been broken down at some point. The then unprotected bone ends will rub against each other. In some cases, this will result in severe movement restrictions and pain. This pain may persist for a long time, and may not be directly related to movement.
Due to the fact that symptoms may vary widely, it is very difficult to determine the progression. While some patients never experience any pain and only suffer from minor movement restrictions, others may suffer from severe pain and restrictions. Others will experience symptoms that disappear on their own after a while. Gonarthrosis does not necessarily need to cause problems, even for a person who is genetically predisposed.
A decrease in the cartilage in the knee joint due to arthrosis cannot be reversed, but the affected person can very effectively influence the rate of progression of the disease and the manifestation of symptoms. Among other things, reducing obesity and remaining physically active may strengthen the knee muscles and greatly delay the progress of the disease, and thus reduce movement restrictions and pain.
Gonarthrosis can manifest itself in very different ways. The symptoms are initially indicated as mild and transient pain during exercise. They may develop to persistent and severe pain, movement restrictions, and loss of stability.
Diagnosis: gonarthrosis
The initial assessment is made based on the patient’s medical history. The aim is to determine whether there is a history of an illness or an injury. This step should also help to rule out other diseases that could be the cause of the complaints. The patient is then subjected to a clinical examination. Mobility and stability tests should provide more information on leg malfunctions. Function tests are used to test mobility and pain reactions via targeted manual manoeuvres by the physician.
Imaging techniques can also be used to examine the condition of the knee joint, and the cartilage in particular. X-rays can clearly show major damage caused by wear. Particular attention is paid to the size of the joint space. The smaller it is, the more advanced the gonarthrosis. X-rays can also detect a deformation (osteophytes) in the articular surfaces (Theiler 2002).
Arthrosis is generally classified into 5 different degrees of severity according to the Kellgren-Lawrence score (Lützner et al. 2006):
- Grade 0: no signs of arthrosis
- Grade 1: minor joint space narrowing
- Grade 2: minor joint space narrowing and slight irregularities in the articular surface
- Grade 3: pronounced narrowing of the joint space and substantial irregularities in the articular surface
- Grade 4: pronounced narrowing of the joint space and deformation/necrosis (death of bone cells) in the joint parts

Treatment of gonarthrosis
Various treatment options are available for treating gonarthrosis. Removal of the cartilage from the knee joint can be prevented conservatively by exercise and physiotherapy. This mainly includes exercises to strengthen the protective and stabilising knee muscles. Orthoses and shoe inserts can also be used for support. Medication can also be used to alleviate pain and prevent inflammation.
If the amount of cartilage in the knee joint has already decreased to a significant degree, surgery is another way of slowing down the progression of gonarthrosis and counteracting its symptoms. Surgical treatments, such as implanting an artificial knee
joint or correcting bones (osteotomy) in deformed legs, are serious and should only be considered if conservative therapy has been unsuccessful and the pain is persistent and very severe.
Rehabilitation for patients with gonarthrosis
Rehabilitation for gonarthrosis is a key treatment phase. It is crucial for restoring the knee function and relieving symptoms. Extensive physiotherapy is not only essential in the conservative treatment of gonarthrosis, but also after surgery. The weakened knee must be slowly rebuilt through adapted exercises. Additional electrotherapy may significantly accelerate the healing process.

Functional electrical stimulation helps rebuild muscles weakened by arthrosis.
Electrotherapy for patients with gonarthrosis
Another rehabilitation option is functional electrical stimulation. The electrical stimulation of muscles can provide important support in every phase of rehabilitation.
By selecting different programmes, the stabilising and protective muscles on the knee joint can be stimulated to prevent muscle atrophy (muscle wasting), which is caused by an adaptive posture in everyday life or after surgery.
Stimulation of an isolated muscle with simple muscle strengthening programmes, the combined stimulation of several muscles in a specific motion sequence, or EMG-triggered stimulation may simplify and accelerate the treatment of gonarthrosis. Pain can also be treated using TENS programmes.
Sport and gonarthrosis
Sport can contribute to increasing well-being, reducing pain and restoring the functioning of the body. However, the indication of gonarthrosis during sport is subject to certain restrictions and requires increased caution in order not to cause a deterioration of the condition.
While low-impact sports, such as swimming or cycling, may reduce pain, high-impact sports (stressful to the joints), such as football or tennis, may contribute to a deterioration of the condition. Overall, however, sport can be very useful for preventing knee complaints.
Comfortable, well-cushioned footwear should be worn to avoid further stress to the knee. Reducing obesity can also counteract gonarthrosis.
If you are interested in continuing education on functional electrical stimulation and wish for a STIWELL® training directly at your institute or online, please contact us
Find out how functional electrical stimulation with the STIWELL® can be used to treat gonarthrosis (knee arthrosis).
Kiselev, J. (2008). Evidenz von Physiotherapie bei Gonarthrose. physioscience, 4(03), 107-119.
Theiler, R. A. (2002). Epidemiologie, Diagnose und Differentialdiagnose, Abklärung und Dokumentation. Schweiz Med Forum, 23, 555-561.
Stöve, J. (2018). S2k-Leitlinie Gonarthrose. Online: https://www.awmf.org/uploads/tx_szleitlinien/033-004l_S2k_Gonarthrose_2018-01_1.pdf (abgerufen
am 7.1.2019)
Lützner, H. J., Kirschner, S., & Günther, K. P. (2006). Epidemiologie und Diagnostik der Gonarthrose. OP-JOURNAL, 22(03), 142-147.

