Stroke (apoplexy)
A stroke (apoplexy) is a medical emergency. It involves sudden vascular damage to the brain and must be treated immediately.
Read more about strokes in this article: What happens during a stroke? What are the symptoms, consequences, and treatment options? Which rehabilitation options are available? And much more...
What is a stroke?

A stroke (ICD 10 code: I60-I64, G45, I69) is sudden brain damage with symptoms such as a severe headache, paralysis, dizziness or speech disorder. It is caused by a circulatory disorder. This may be due to ischaemia (cerebral infarction) or haemorrhage (cerebral haemorrhage) (Rohkamm 2009).
With the number of new cases (incidence) of the disease affecting 16.9 million people worldwide each year, strokes cause a loss of 102 million healthy years of life (Feigin et al. 2014) as 90% of those affected experience limitations (Williams et al. 1999).
Symptoms of a stroke
The respective symptoms depend on the location and severity of the stroke. Symptoms are often accompanied by severe, non-specific nausea and headaches. In the event of a sudden occurrence of one or more of these symptoms, rapid action is of major importance (European emergency phone number 112):
- Paralysis or paresis on one side (hemiparesis or hemiplegia): for example, on one side of the body, one arm or leg, one half of the face: Facial nerve palsy – e.g. drooping corner of the mouth
- Numbness on one side (sensory disorder)
- Coordination disorders
- Language or speech disorders (aphasia or dysarthria): e.g. slurred speech, difficulty finding words, loss of ability to speak
- Vision problems or blindness (e.g. restricted vision, double vision)
- Dizziness, nausea, balance disorders
- Difficulty swallowing (dysphagia)
- Unconsciousness, confusion or other cognitive impairment
- Hemispatial neglect
- etc.
How can one recognise a stroke?

A stroke may cause a wide variety of symptoms, which can occur in different combinations. For this reason, a layperson often cannot tell if it is a stroke. The FAST test can be helpful in the event of a suspected stroke and should thus be performed by the first responder.
FAST - rapid test in the event of a suspected stroke
F - face: Ask the affected person to smile. Can you detect facial paralysis on one side?
A - arms: Ask the person to close his or her eyes and then stretch both arms in front at the same time, while turning the palms upward. (In the event of paralysis, the patient will not be able to lift one arm, or the arm will drop or twist.)
S - speech: Ask the person to repeat a simple sentence. (In the event of speech disorders, this will not be possible or will be difficult; with speech disorders, the pronunciation will be slurred.)
T - time: Call the emergency services immediately if any of these symptoms are present. Many strokes can be detected with the help of this rapid test. Inform the emergency services that you suspect a stroke.
Warning signs of a stroke
During a transient ischaemic attack (TIA), one or more symptoms usually only appear for a few minutes, and then disappear without causing permanent damage. This makes it all the more important to take this warning sign seriously and to clarify the cause of it. This may prevent a possible stroke. The first stroke is not always a TIA or a minor stroke. Larger vascular occlusions are also possible. In this case, a warning sign may also be a temporary sudden loss of vision in one eye (amaurosis fugax).
First aid for a stroke - What should be done in an emergency?
‘Time is brain!’
If you suspect a stroke, call emergency services immediately (Europe-wide number 112) and perform the FAST test. Answer the questions of the emergency control centre carefully, and give a BRIEF description of the situation:
- What symptoms does the affected person have?
- When did the symptoms start?
- How did the symptoms develop?
- What medications does the patient take? (In particular, do they take any blood thinners?)
The emergency control centre may give you different instructions, depending on the situation, such as:
- Lift the upper body by 30°
- If the person is unconscious, place him/her in the recovery position
- etc.
Important: Do not leave the affected person alone and calm him/her down. Do not give the affected person anything to eat or drink (swallowing disorder), and do not administer blood thinners (aspirin, etc.) if unauthorised to do so.
Apart from a severe headache and nausea, a wide range of symptoms can be seen during a stroke, such as weakness in arms or legs, numbness, dizziness, speech disorders, or a drooping corner of the mouth. If you suspect a stroke, notify emergency services immediately!
Diagnosis: stroke
Once the first responder has notified the emergency services, the affected person must be taken to a specialised hospital as soon as possible, ideally one equipped with a stroke unit. This is important to ensure that specialist stroke treatment can begin. Immediate medical treatment increases the chances of saving the affected person's life, and may prevent permanent disability and irreparable damage.
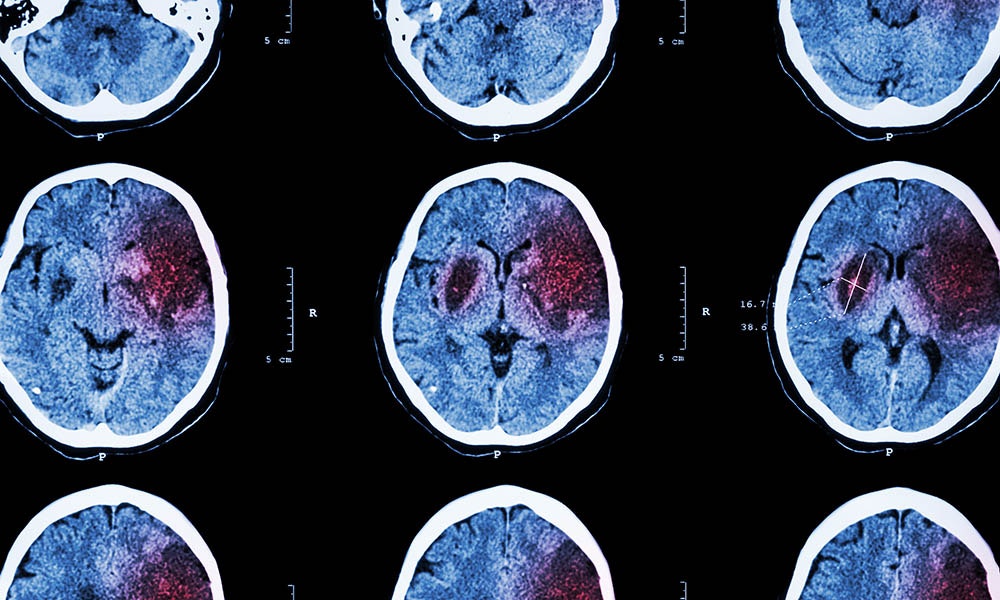
To ensure targeted therapy, it is necessary to establish whether the patient suffers from reduced blood flow or cerebral haemorrhage. This is usually done by imaging techniques, such as computed tomography (CT) and/or magnetic resonance imaging (MRI) of the brain.
Is the stroke mild or severe?
The National Institutes of Health Stroke Scale (NIHSS) is used to clinically assess the severity of a stroke. In addition to imaging techniques, NIHSS is an important parameter for the determination of acute treatment, and for follow-up documentation. This scale assesses the extent of the various symptoms. A low total score indicates a mild stroke, while a higher score indicates a severe stroke.
Causes of a stroke
During a stroke, the blood supply to the brain is impaired. Depending on the duration and extent of the stroke, cells in the affected area may be damaged or may even die. Depending on the severity and localisation of the stroke, it may cause dysfunction or even death.
What are the specific causes of a stroke?
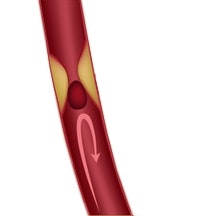
Reduced blood flow (ischaemic stroke, cerebral infarction)
Occlusion of blood vessels that supply the brain means that parts of the brain are no longer properly supplied with blood. This may be due to vascular calcification (atherosclerosis), blood clots (clots that form in the heart and reach the brain), or
vascular inflammation. This form occurs in about 80 percent of cases (Donnan et al. 2008).
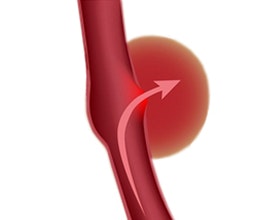
Brain haemorrhage (haemorrhagic stroke)
A cerebral haemorrhage involves blood flowing into the surrounding brain tissue. The resulting pressure may cause additional damage to unaffected brain areas. This intracerebral or extracerebral haemorrhage may be caused by high blood pressure (hypertension), coagulation disorder, vascular inflammation (vasculitis), tumours, or poorly tailored pharmacological treatment with blood thinners (anticoagulants).
A stroke disrupts the blood supply to the brain (due to reduced blood flow or a brain haemorrhage). The diagnosis is made by means of imaging techniques (CT, MRI), in addition to the clinical neurological examination.
Therapy/acute treatment for a stroke
It is crucial to improve blood circulation (or to stop the bleeding) as soon as possible in order to minimise damage, even in border areas, because ‘time is brain’. A suspected stroke should always be diagnosed as soon as possible, so that targeted treatment can be started immediately. There are various treatment options, depending on the severity, cause, and the time window.
- If a brain vessel is blocked by a blood clot (reduced blood flow) , pharmacological thrombolytic treatment is often applied to dissolve the clot. Another option is thrombectomy, where the blood clot is aspirated through a catheter.
- In the case of a brain haemorrhage , the priority is to stop the bleeding. Furthermore, the too high blood pressure usually has to be lowered by medication. Surgery may be necessary if a larger amount of blood has leaked into the surrounding brain tissue.
Treatment methods for a stroke vary from patient to patient, and must be assessed individually by the patient’s physician. It is also crucial to treat risk factors. The text below provides more information about potential risk factors.
Risk factors for a stroke
There are a variety of risk factors for a stroke, only some of which can be influenced. If some of them apply to you (high blood pressure, hypercholesterolemia, etc.), DO NOT try to treat them on your own. Seek medical attention.
What increases the risk of a stroke?
- Old age
- Genetic predisposition (family history)
- Previous history of stroke
- Arteriosclerosis: This is facilitated by high cholesterol, diabetes mellitus, high blood pressure (hypertension), and smoking.
- Heart disease (atrial fibrillation, heart valve disease, etc.)
- Patent foramen ovale (PFO)
- Lack of exercise, severe obesity, unhealthy diet
- Stress
- Heavy alcohol consumption
- Birth control pills
- etc.
Consequences of a stroke
According to the World Stroke Organization, a stroke is one of the leading causes of long-term disability worldwide.
A stroke may have consequences of varying severity and may cause different impairments for the life of an affected person, depending on which brain areas were affected by the reduced blood flow or cerebral haemorrhage, for how long, and to what extent, and the level of severity of the initial symptoms.
Chances of recovery
As a rule, symptoms improve due to self-healing processes in the body (spontaneous remission) and training. The extent of improvement depends on various factors that must be considered individually for each patient.
How long does the patient stay in hospital?
The average length of stay in the acute care hospital is approx. 2 weeks. The affected person may then be referred to a rehabilitation clinic or may be allowed to go home (with or without outpatient therapy).
Life expectancy
Each person must also be considered individually in this respect. Young people with no residual symptoms tend to have a good prognosis, provided the cause has been treated and risk factors have been remedied. Conversely, the risk increases if no cause
can be found and/or the risk factors are not addressed. However, with medical standards improving, the mortality rate has been generally decreasing for years (Feigin et al. 2014).
The sooner the blood circulation is improved (or bleeding is stopped), the more likely the secondary damages can be minimised after a stroke. Acute treatment can be either pharmacological or surgical.
Rehabilitation after a stroke
With its ‘1 in 6’ campaign, the World Stroke Organization illustrates the current situation: Every six seconds, a person's quality of life is changed forever. He or she will live with a permanent physical disability/limitation following a stroke. To reduce the risk of permanent physical impairments after a stroke, the affected person should receive appropriate medical treatment as well as adequate therapy and rehabilitation as soon as possible.
The consequences of brain damage are wide-ranging (stroke symptoms) and require individual therapy. Various rehabilitation measures can restore impaired body functions completely or to some extent. This is made possible, on the one hand, by functional
compensation and, on the other, by structural and functional changes in the brain (neuroplasticity).
Goal of rehabilitation
The goal of rehabilitation is to enable the affected person to recover skills that are necessary for an independent and self-determined life. This includes the basic activities of daily life, as well as participation in a social and professional life.
In some cases, rehabilitation can only reduce dependence and discomfort due to the severity of the stroke. The affected person often requires support in everyday life. It is important to identify challenges and find ways to overcome them and, if necessary,
to use appropriate aids or other therapeutic measures.
Early rehabilitation – long-term rehabilitation
The earlier the appropriate rehabilitation (=restoration) is started, the better for the success of the therapy. For this reason, early rehabilitation should already be started in the hospital. A multidisciplinary, coordinated team of therapists can carry out activating measures in nursing care, exercises to increase mobility as well as speech and swallowing exercises with the patient at an early stage. In therapy today, the activities of daily life (ADL) are often practiced according to the principles of the motor learning process in order to find back to an independent life step by step.

The type of rehabilitation measures to be applied on a regular basis and for an extended period depends on the type of limitation.
In most cases, an individually tailored therapy plan includes many different therapeutic procedures from a range of specialist fields (physiotherapy, occupational therapy, speech therapy, biofeedback, electrical stimulation, etc.).
Motor learning
Motor learning focuses on the restoration of movement skills after an injury. There is no framework that needs to be followed, but we know that certain factors have a major impact on the learning process, and thus on long-term therapeutic success. The following aspects of the learning process are of major relevance:
- active exercising (Hauptmann & Müller 2011)
- actions oriented towards objectives and everyday activities (Hauptmann & Müller 2011)
- random selection of activities (Hauptmann & Müller 2011)
- variability of exercises (Mulder 2007)
- optimal feedback (Mulder 2007)
- shaping (Woldag 2011)
- repetition (Lang et al. 2007, 2009; Hauptmann & Müller 2011)
- motivation (Wulf 2010)
- enriched environment (Mehrholz 2008)
The recommended therapy frequency is 5 units with exercise sequences of 30-45 minutes per week (Platz 2011).
Rehabilitation after a stroke should begin as early as possible and should be tailored to the individual patient. The regular application of different measures as well as the support provided by relatives and care personnel contribute to the success of the therapy.
What are the possible therapy options for rehabilitation after a stroke?
There are, among others, the following therapy options that may help improve motor functional deficits and activities:

Physiotherapy after a stroke

Physiotherapy
The physiotherapist draws up an individually tailored therapy plan based on the existing functional deficits and malfunctions. The re-learning of movements or alternative compensation strategies and the use of aids contribute to the ability to master everyday life independently again.
Regular exercises to improve balance, coordination, body awareness and spasticity (increased muscle
tension) as well as for muscle building and endurance training are carried out here. The goal is to maintain or improve patients' mobility , so that they can regain optimal levels of physical independence in everyday life. Relatives are often
involved in physiotherapy.
Occupational therapy
Occupational therapists help patients to use everyday-relevant aids in order to compensate for disability-related limitations. They teach patients to perform motor functional activities and practical tasks (such as washing, dressing, shopping), which are intended to encourage patients' own activities.
The affected persons should regain the maximum level of independence in their daily lives. Occupational therapists also advise the relatives and offer guidance and assistance on how to support those affected.
Speech therapy
Speech disorders and dysphagia can be treated with the help of a speech therapist. Speech therapy helps to improve the communication skills, speech quality, clarity of pronunciation, and independent eating of those affected.
The treatment also focuses on the paralysis of facial muscles (facial nerve palsy). The therapy is adjusted to the deficits of the individual patient. Relatives are also given information on how to handle these disorders.


Biofeedback
Mobility impairments can be treated by means of biofeedback. An electromedical device reports the movements back to the affected person, using both visual and acoustic signals. This helps the user to be aware of his/her movements. The result is cognitive re-learning of the movement or conscious tensioning of the affected muscles in the event of paralyses (pareses).
Symptom-oriented biofeedback training, which may be combined with muscle-controlled electrotherapy, is an effective therapeutic tool that can be used to supplement the treatment of neurological damage. Patients can apply it over the course of rehabilitation or as controlled home therapy after rehabilitation.
Electrotherapy
Functional electrical stimulation can be optimally used for rehabilitation after a stroke, in addition to the conventional exercise therapy, for the re-learning of everyday functions. Upon completion of the acute treatment, electrotherapy can already be started in the clinic. It should then be applied regularly for a longer period, on an outpatient or inpatient basis, as part of a specified treatment plan.
Patients can also rent some electrotherapy devices for home therapy once they have been briefed by a physician/physiotherapist on how to use them (for example, the STIWELL®, see home-based therapy). Electrotherapy can thus be applied in all phases of neurological rehabilitation. The effectiveness of electrotherapy has been demonstrated in several studies.
How does electrotherapy help after a stroke?
A stroke may interrupt the signal transmission from the brain to the muscle via the spinal cord and the neural pathways if the respective brain areas or nerve cells are damaged. As a result, the affected muscles are not stimulated or are stimulated less
often, and the muscle mass decreases (muscle atrophy). Electrotherapy may help to build up the flaccid muscles at the start of the therapy. Motion sequences can be re-learned with the help of the EMG-triggered multi-channel electrical stimulation
(EMG MES) and the biofeedback. Targeted and reproducible functions should be practised and repeated frequently for the therapy to be successful.
Electrical stimulation can be used in all phases of neurological rehabilitation after a stroke. It serves to strengthen the muscles and to train everyday functions.
If you are interested in continuing education on functional electrical stimulation and wish for a STIWELL® training directly at your institute or online, please contact us
Prevention: stroke
How can I reduce the risk of (another) stroke?
It is crucial to minimise the risk factors, and to find out and correct the cause of the stroke. There are a variety of risk factors for a stroke, only some of which can be directly influenced. If some of them apply to you (high blood pressure, hypercholesterolemia,
etc.), DO NOT try to treat them on your own, but seek medical advice! As a rule, it is beneficial to lead an active life with lots of exercise and a healthy diet. Regular visits to the physician will help you to become aware of possible diseases in
good time and to take the right steps.
Find out how functional electrical stimulation with the STIWELL®
can help you re-learn movements after a stroke!
Donnan, G. A., Fisher, M., Macleod, M., Davis, S. M. (2008). Stroke. The Lancet, 371 (9624), 1612-1623.
Feigin, V. L., Forouzanfar, M. H., Krishnamurthi, R., Mensah, G. A., Connor, M., Bennett, D. A., ... & O'Donnell, M. (2014). Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. The Lancet, 383(9913), 245-255.
Hauptmann, B. & Müller, C. (2011). Motorisches Lernen und repetitives Training. In: Nowak, D. (Hrsg.) Handfunktionsstörungen in der Neurologie. Berlin Heidelberg: Springer Verlag, 214-223.
Lang, C. E., MacDonald, J. R., & Gnip, C. (2007). Counting repetitions: an observational study of outpatient therapy for people with hemiparesis post-stroke. Journal of Neurologic Physical Therapy, 31(1), 3-10.
Lang, C. E., MacDonald, J. R., Reisman, D. S., Boyd, L., Kimberley, T. J., Schindler-Ivens, S. M., ... & Scheets, P. L. (2009). Observation of amounts of movement practice provided during stroke rehabilitation. Archives of physical medicine and rehabilitation, 90(10), 1692-1698.
Mehrholz, J. (2008). Frühphase Schlaganfall. (1. Aufl.). Stuttgart: Georg Thieme Verlag.
Mulder, T. (2007). Das adaptive Gehirn. Stuttgart: Georg Thieme Verlag.
Platz, T. (2011). Rehabilitative Therapie bei Armlähmungen nach einem Schlaganfall. Patientenversion der Deutschen Gesellschaft für Neurorehabilitation. Bad Honnef: Hippocampus Verlag.
Rohkamm, R. (2009). Taschenatlas Neurologie. (3. Aufl.). Stuttgart: Georg Thieme Verlag.
Williams, G. R., Jiang, J. G., Matchar, D. B., & Samsa, G. P. (1999). Incidence and occurrence of total (first-ever and recurrent) stroke. Stroke, 30(12), 2523-2528.
Woldag, H. (2011). Shaping. In: Nowak, D. (Hrsg.) Handfunktionsstörungen in der Neurologie. Berlin Heidelberg: Springer Verlag, 223-224.
Wulf, D. (2010). Motorisches Lernen. In: Hüter-Becker, A., Dölken, M. (Hrsg.). Physiotherapie in der Neurologie. (3.Aufl.). Stuttgart: Georg Thieme Verlag, 41-72.

