Hip arthrosis
Hip arthrosis, also called coxarthrosis, is a disease of the hip joint. Protective cartilage material breaks down on both the femoral head and the acetabulum. The consequences initially manifest themselves as minor movement restrictions, which may subsequently worsen and cause severe pain.
Learn more about hip arthrosis in this article. What exactly is hip arthrosis and what are its symptoms? What causes hip arthrosis? What are the possible treatments and therapies? And much more …
What is hip arthrosis?
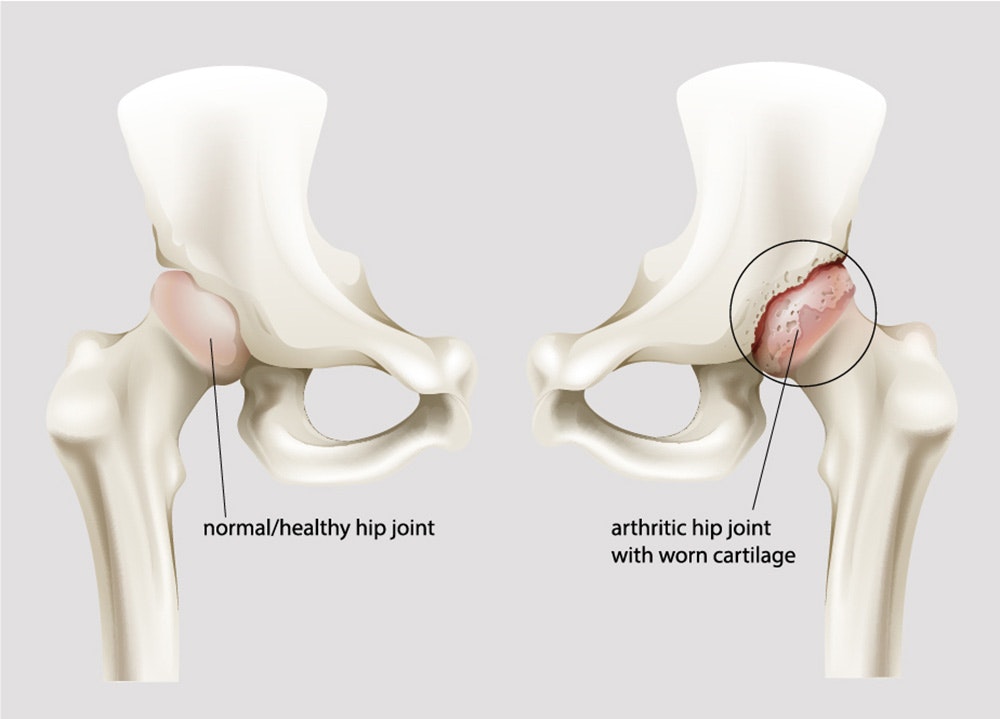
Hip arthrosis (ICD code M16) is a form of athrosis - a disease in which cartilage material in the joints deteriorates due to wear. Hip arthrosis (coxarthrosis) is a disease of the hip joint, caused by wear of the cartilage on the head of the femur (os femoris) and the joint socket of the hip bone (os coxae).
The cartilage stabilises the joint, and protects it against damage due to friction against the bone. A deterioration of the cartilage mass may cause restricted movement and severe pain.
There are two types of arthrosis. Primary arthrosis is a genetic form of the disease. Symptoms may not necessarily be apparent in a patient with primary arthrosis. This form of the disease may last a lifetime without being noticed. Secondary arthrosis is caused by external impact, such as injuries due to accidents, misaligned legs (knock knees/bow legs), or constant stress in everyday life.
Arthrosis is often mistaken for arthritis. Arthritis is a generic term for inflammatory joint diseases. These include, for example, infection-related arthritis and rheumatoid arthritis. In some cases, however, hip arthrosis may also cause inflammation and thus develop into arthritis.
In Germany, approx. 6% of people over the age of 40 suffer from hip arthrosis. Up to the age of 75, hip arthrosis affects women and men more or less equally. From then on, women are more likely to be affected. From the age of 75, the prevalence increases to approx. 17% for women and approx. 16% for men. However, hip arthrosis is generally less common than gonarthrosis (Endres et al. 2018).
Causes of hip arthrosis
The causes of hip arthrosis are extremely diverse, and are usually due to a combination of several factors. However, the common factor is a metabolic disorder in the cartilage. Cartilage degradation processes predominate and gradually lead to an exposure of the bone. If one bone rubs against another bone, the body reacts by producing bone material to counteract the breakdown. This causes bone deformity, and resulting limitations in mobility as well as pain (Rabenberg 2013).
Repairing the damage to the cartilage is particularly difficult for the body. Cracks in the cartilage material are usually irreversible.
The following factors may promote the development of hip arthrosis or are the cause of hip arthrosis:
- Genetic predisposition
- Age-related wear
- Hip alignment problems
- Hip diseases
- Severe obesity
- Heavy physical exertion
- Sport
- Injuries
- Hip impingement
Hip impingement occurs if the acetabulum and the femoral head do not fit completely together. The reasons for this are unclear. A genetic predisposition usually plays a role.
Risk factors for hip arthrosis
In addition to genetic factors and age, the other particular risk factor is overloading of the hip joint due to obesity and permanent physical workloads.
In most cases, hip arthrosis is caused by a combination of various factors. Genetic predisposition, obesity, and age-related wear are among the most common causes.
Symptoms of hip arthrosis
In most cases, hip arthrosis causes pain and restricted movement in the hip joint. In the early stages of the disease, however, there may be no noticeable symptoms. Those affected usually feel only minor pain when walking or getting up from a sitting position. These complaints often disappear on their own after a short time. As the disease progresses, the pain spreads, sometimes down to the knees, and movements such as bending or climbing stairs become more difficult and painful.
Rapidly progressing hip arthrosis means that all of the cartilage material will break down in the foreseeable future. The then unprotected bone ends will rub against each other. This usually causes severe movement restrictions and pain.
The breakdown of the cartilage material due to arthrosis cannot be stopped. However, reducing obesity and increasing physical activity may help strengthen the muscles and reduce movement restrictions and pain.Typical symptoms of hip arthrosis:
- hip joint pain
- groin pain
- limping
- restricted mobility
- pain at rest
Diagnosis: hip arthrosis
The initial aim is to determine whether there is a history of an illness or injury. This step can also help to rule out other diseases that could be the reason for the complaints.
The patient is then subjected to a clinical examination. Mobility tests and functional tests provide information on mobility and pain reactions.
In the next step, imaging techniques are used to determine the condition of the hip joint, especially the cartilage.

Particular attention is paid to the size of the joint space. The smaller the joint space, the more advanced the hip arthrosis. X-rays can also detect a deformation (osteophytes) in the articular surfaces (Theiler 2002). In rare cases, ultrasound,
computed tomography, or magnetic resonance imaging may also be used for a more precise diagnosis. A blood analysis can also be performed to distinguish between arthritis and arthrosis, which is sometimes difficult.
Arthrosis can be classified by means of radiological diagnostic tests and divided into 5 grades according to Kellgren and Lawrence (Kellgren & Lawrence 1957):
Grade 0: no signs of arthrosis
Grade 1: minor joint space narrowing
Grade 2: minor joint space narrowing and slight irregularities in the articular surface
Grade 3: pronounced narrowing of the joint space and substantial irregularities in the articular surface
Grade 4: pronounced narrowing of the joint space and deformation/necrosis (death of bone cells) in the joint parts
Treatment of hip arthrosis
The treatment of hip arthrosis is usually conservative at first, depending on the stage of the disease. This conservative treatment primarily involves movement therapy or physiotherapy to strengthen the muscles in the hip joint. Targeted exercises can also improve mobility and balance, and thus slow down the progress of arthrosis and relieve pain. Additional physiotherapy or massages can relieve tension and pain. Pharmacological treatment with anti-inflammatory painkillers can also be used to relieve pain.
If the hip arthrosis is due to a misalignment, orthopaedic shoe inserts can help counteract this and alleviate symptoms.
Sports should not be avoided for fear of deterioration. Regular physical activity promotes blood circulation and helps joint mobility, thus contributing to the patient’s improvement. However, care should be taken to choose sports that do not expose the hip joint to excess stress. Such suitable sports would include water aerobics, swimming, cycling, or simple walks.
If the amount of cartilage in the hip joint has already decreased to a significant degree, surgery is another way of slowing down the progression of hip arthrosis and of effectively counteracting its symptoms. Implanting an artificial hip joint is a serious procedure and should only be considered if conservative therapy has been unsuccessful and the pain is persistent and very severe. Surgeries in the form of minimally invasive procedures, such as hip arthroscopy, may help resolve symptoms already at an early stage of hip arthrosis.

Hip arthrosis is usually treated using conservative therapies. Pain can also be treated with medication.
Rehabilitation after hip arthrosis
Special attention should be paid to rehabilitation for hip arthrosis. The rehabilitation focuses on reducing arthrosis-related symptoms, pain, and dysfunctions, and improving the patient’s quality of life, which is often severely affected. Regular
physical and occupational therapy may significantly slow down the progression of arthrosis, and may greatly reduce the limitations in everyday life. Specially coordinated exercise programmes can help strengthen the supporting muscles around the hip
joint and thus relieve symptoms. Training on aids (such as rollators) and nutrition advice are also part of a thorough rehabilitation (Rabenberg 2013).
Sport & arthrosis
While exercise generally has a proven positive effect on hip arthrosis, exercise must still be performed subject to some restrictions. Low-impact sports, such as swimming or cycling, may help reduce pain. On the other hand, high-impact sports (stressful
to the joints), such as football or tennis, may contribute to a deterioration of the condition. Overall, however, sport can be very useful for preventing hip complaints.
Electrotherapy for patients with hip arthrosis
Functional electrical stimulation represents an increasingly important and growing aspect of rehabilitation. Various programmes include patient-specific settings. The stabilising and protective muscles on the hip joint can be stimulated to prevent muscle atrophy (muscle wasting), which is caused by an adaptive posture in everyday life or after surgery.
The isolated stimulation of a muscle with simple muscle strengthening programmes, the combined stimulation of several muscles in a specific motion sequence, or EMG-triggered stimulation may simplify and accelerate the treatment of hip arthrosis. Electrotherapy thus provides valuable support in every phase of the treatment.
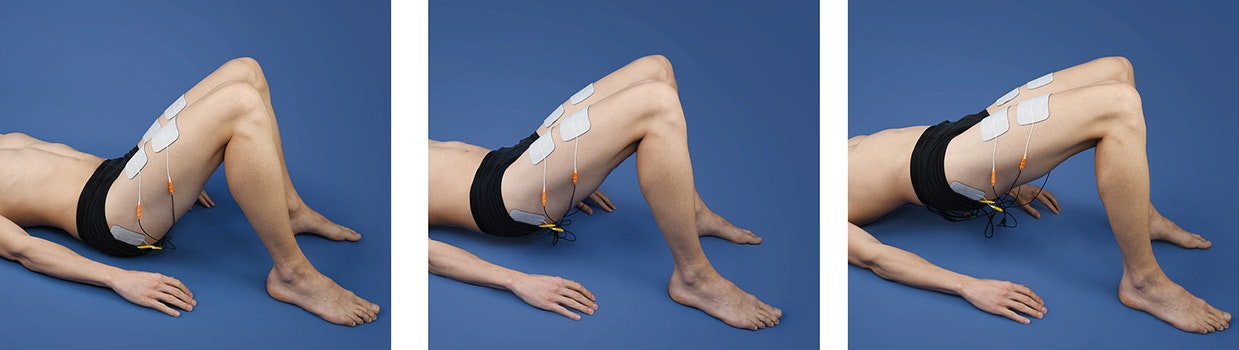
Functional electrical stimulation (FES) for muscle strengthening in patients with hip arthrosis
Hip replacement in the case of hip arthrosis
Hip replacement is a surgical procedure in which a hip joint that has been damaged for various reasons is replaced by an artificial joint. A hip joint replacement or total hip replacement (total hip arthroplasty) is used if conservative therapies do not provide good results.
There are three types of hip prostheses:
- Cementless prosthesis: the artificial joint is clamped or screwed into the bone. It then grows naturally into the bone (in younger patients).
- Cemented prosthesis: the artificial joint is fixed to the bone using bone cement (in elderly patients).
- Hybrid prosthesis: the joint socket is fixed naturally, and the stem of the prosthesis is cemented.
Surgery takes 2 to 4 hours and is usually performed under a general anaesthetic. The patient can often leave the hospital the next day. A total hip replacement will last approximately 15 to 20 years on average before it needs to be replaced. Good
healing and the immediate start of physiotherapy are important in ensuring that the new joint is mobilised.
If you are interested in continuing education on functional electrical stimulation and wish for a STIWELL® training directly at your institute or online, please contact us
Find out how functional electrical stimulation with the STIWELL® can be used to treat hip arthrosis.
Endres, H., Schneider, O., Scharf, H. P., Kaufmann-Kolle, P., Knapstein, S., Hermann, C., ... & Flechtenmacher, J. (2018). Koxarthrose–Epidemiologie und Versorgungsrealität–Versorgungsdatenanalyse von 2, 4 Millionen Versicherten der AOK Baden-Württemberg ab 40 Jahren. Zeitschrift für Orthopädie und Unfallchirurgie, 156(06), 672-684.
Kellgren, J. H., & Lawrence, J. S. (1957). Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases, 16(4), 494.
Rabenberg, M. (2013). Gesundheitsberichterstattung des Bundes, Themenheft 54 "Arthrose." Robert Koch-Institut, 10-14.
Theiler, R. A. (2002). Arthrose. Epidemiologie, Diagnose und Differentialdiagnose, Abklärung und Dokumentation. Schweiz Med Forum, 23, 555-561.

