Plegias
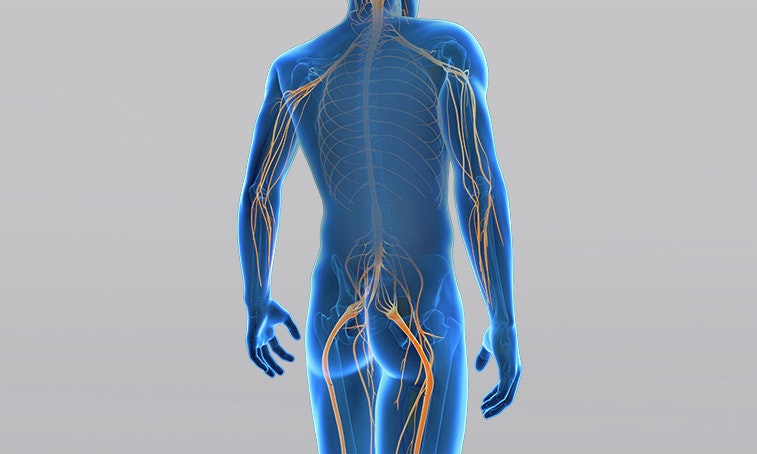
Plegia refers to the complete paralysis of one or more muscles, which cannot be tensed anymore. It is caused by nerve damage in the brain (upper motor neuron/central damage) or further on in the body (lower motor neuron/peripheral damage).
What are the forms of plegia and what treatment or therapy methods are available? Definition, numbers, causes, and diagnosis at a glance ...
What is a plegia?
Plegia, or paralysis, is a complete paralysis of skeletal muscles. An incomplete paralysis is called a paresis. A plegia is caused by damage to one or more nerves that travel from the brain to the muscle and initiate movements. Nerves can get damaged along their course in the upper or lower motor neuron, i.e. in the brain, in the spinal cord, or in the body.
Plegias can be classified by the location of damage or by the affected limb.
Depending on the location of nerve damage, either in the upper or in the lower motor neuron, plegias are classified as central or peripheral. The lower motor neuron extends from the anterior horn cell of the spinal cord to the neuromuscular junction of the muscle. An injury in the lower motor neuron is called a peripheral plegia. Peripheral plegias may affect one or more nerves (plexus paresis).
The upper motor neuron runs from the brain to the anterior horn cell of the spinal cord. If damage occurs in this part of the nerve, it is called a central plegia.

Central plegias are classified according to the affected limb:
- Monoplegia
The complete paralysis affects only one limb, e.g. monoplegia of one arm.
- Paraplegia
Both legs are completely paralysed; upper limbs (arms) are not affected.
- Hemiplegia
Arm and leg of one side of the body are completely paralysed.
- Quadriplegia (tetraplegia)
It involves a complete paralysis of all four limbs (arms and legs), and control over the torso and head is impaired.
In the case of central damage, the paralysis always affects the side opposite to the affected cerebral hemisphere. This means that damage to the right cerebral hemisphere paralyses the left side of the body and vice versa.
Causes of a plegia
Muscle paralysis is caused by damage along the course of the afferent nerve (upper or lower motor neuron). The nerve may be damaged, for example, by bleeding, infarction, inflammation, excessive pressure, or cuts. The conditions which may cause plegias are, for example:
- Stroke
- Traumatic brain injury
- Infantile cerebral palsy (early childhood brain damage)
- Multiple sclerosis
- Tetraplegia
- Herniated disc
- Carpal tunnel syndrome
- Tumours
Especially in the case of central causes, it is rare that only complete plegias, i.e. complete paralyses, occur. In most cases, the clinical presentation is a combination of complete paralyses (plegias) and incomplete paralyses (pareses), as is the case, for example, in tetraplegia with incomplete paralysis (Swiss Paraplegics Association 2012).
Diagnosis: plegia

Imaging techniques such as CT or MRI are used to diagnose a potential central plegia.
Paralyses are evaluated by testing the muscle strength. The clinical testing of muscle strength is carried out via assessments. The most common is the assessment with the help of the Medical Research Council (MRC), where 0 points represent a plegia.
If peripheral nerve damage is suspected, nerve or muscle information can be obtained by measuring nerve conduction velocity (NCV or electroneurography/ENG).
Electromyography (EMG), whereby needle electrodes are stuck into the muscle, enables the computer evaluation to provide an even more precise statement about the muscle condition of patients with injury-related atrophy (muscle wasting).
If clinical symptoms suggest a central cause of plegia, computed tomography (CT) or magnetic resonance imaging (MRI) may provide more information about the damage.
Progress of a plegia
The lack of contraction in the muscle due to the paralysis causes a reduction of muscle mass (atrophy) over time. It also causes abnormalities of the connective tissue (fibrosis) in muscle fibres and increased fat deposits.
Due to the lack of control by the brain in the case of central damage, patients with plegias often also develop spasticity (increased muscle tension) in the course of healing. For example, children with infantile cerebral palsy often have spastic monoplegia, paraplegia, hemiplegia or quadriplegia (tetraplegia). The spasticity in turn causes limited joint mobility, which may result in joint stiffness (contractures).
Rehabilitation for a plegia
In the case of complete paralysis, the cause cannot be corrected by classic physiotherapy, since the paralysed muscle can no longer be activated by the patient himself. This is why therapy with targeted functional electrical stimulation has proven successful. Special current waveforms combined with long pulse duration and low frequencies can address the muscle directly and cause it to contract. This may prevent muscle wasting and abnormalities of connective tissue (Kern et al. 2010), and can support nerve regeneration (Gordon et al. 2016).
Spasticity and joint stiffness, which occur after central paralyses, can be treated by a physiotherapist by means of stretching under weight and active movement exercises. In some cases, spasticity is also treated with botulinum toxin (Botox) injections into the affected spastic muscle groups. The targeted effect of the Botox neurotoxin can be improved by combining it with functional electrical stimulation (Cotoi et al. 2018).
If you are interested in continuing education on functional electrical stimulation and wish for a STIWELL® training directly at your institute or online, please contact us
Find out how functional electrical stimulation with the STIWELL® can be used in the treatment of plegias.
Cotoi, A., Iliescu, A., Foley, N., Mirkowski, M., Harris, J., Dukelow, S., Knutson, J., Chae, J., Miller, T., Lee, A., Janssen, S. & Teasell, R. (2018). EBRSR Evidence-Based Review of Stroke Rehabilitation. Chapter 10. Upper Extremity Interventions, 91.
Gordon, T., & English, A. W. (2016). Strategies to promote peripheral nerve regeneration: electrical stimulation and/or exercise. European Journal of Neuroscience, 43(3), 336-350.
Kern, H., Carraro, U., Adami, N., Biral, D., Hofer, C., Forstner, C., ... & Paolini, C. (2010). Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabilitation and neural repair, 24(8), 709-721.
Schweizer Paraplegiker Vereinigung (2012). Querschnittlähmung. Paradidact SPV Nottwil.

